Will A Heel Spur Cause Pain?
Overview
The term heel spur generally refers more specifically to a heel spur, also known as a calcaneal spur. These calcium growths form around the tendons and ligaments of the foot and eventually become attached to the heel bone. The spurs then continue to grow, piercing the skin of the foot and causing pain and discomfort. When left untreated the spur can continue to grow causing agonizing pain and even immobilizing the patient.
Causes
The cause of heel spurs is excessive strain placed on the plantar fascia over a long period of time, as a result of different factors. These factors include incorrect gait, being overweight, ageing or being in a job that requires a lot of standing on hard floors. It is usually a combination of any of these factors that will bring on the development of heel spurs.

Symptoms
Heel spur is characterised by a sharp pain under the heel when getting out of bed in the morning or getting up after sitting for a period of time. Walking around for a while often helps reduce the pain, turning it into a dull ache. However, sports, running or walking long distance makes the condition worse. In some cases swelling around the heel maybe present.
Diagnosis
Your doctor will review your medical history and examine your foot. X-rays are used to identify the location and size of the heel spur.
Non Surgical Treatment
Ice compresses, stretching exercises, night splint for traction of the leg muscles to stretch the muscle in the back of the leg, and massage of the back of the leg, along with padding and heel cushions are also things that you can do at home. The number one recommendation for relief of heel pain is wearing good shoe gear. Good shoe gear usually consists of a sturdy, solid shoe. Heel pain is not relieved by a soft, ill supported shoe. Shoes such as Nike, K-Swiss, and Avia are the best shoes for this condition. Custom orthotics are highly recommended. Physical therapy is another way physicians treat this condition. Ice packs, muscle stimulation, ultra sound, paraffin baths, and the new Plantar Fascitis Night Splint are also helpful. If all these conservative measures fail to relieve the pain, then surgery is indicated. The newer minimal incision surgeries such as the Endoscopic plantar fasciotomy surgery is extremely beneficial for this condition, and for earlier ambulation, the use of the newer Cast Walking Boot is recommended.
Surgical Treatment
More than 90 percent of people get better with nonsurgical treatments. If conservative treatment fails to treat symptoms of heel spurs after a period of 9 to 12 months, surgery may be necessary to relieve pain and restore mobility. Surgical techniques include release of the plantar fascia, removal of a spur. Pre-surgical tests or exams are required to identify optimal candidates, and it's important to observe post-surgical recommendations concerning rest, ice, compression, elevation of the foot, and when to place weight on the operated foot. In some cases, it may be necessary for patients to use bandages, splints, casts, surgical shoes, crutches, or canes after surgery. Possible complications of heel surgery include nerve pain, recurrent heel pain, permanent numbness of the area, infection, and scarring. In addition, with plantar fascia release, there is risk of instability, foot cramps, stress fracture, and tendinitis.
Prevention
In 2002, researchers attempted to compare the effects of various running techniques on pronation and resulting injuries like stress fractures and heel spurs. They suggested that it is possible to teach runners to stride in such a way as to minimize impact forces. One way is to lower running speed. Another is to take longer rest periods following a run.
Bursitis Foot Signs And Symptoms
You might be suffering from Achilles bursitis if you have sharp pain at the back of your heel. You have lump on the back of your heel. You have loss of range of motion walking and the pressure for shoes causes you to limp and you have weakness in your leg. You have warmth, redness and swelling on the heel. If any of those statements are true for you or you're suffering from on-going pain in your heel then you might have an injury called "retrocalcaneal bursitis". Many people don't know that Achilles bursitis is a very real injury affecting the bursa sac in your ankle. It can happen to anyone who regularly puts stress with repetitive movements as part of your job, sports related activities, acute trama to the ankle/foot and/or aging weakness the tissue around the ankle and the bursa.
Causes
Posterior heel pain can come from one of several causes. When a physician is talking about posterior heel pain, he or she is referring to pain behind the heel, not below it. Pain underneath the heel, on the bottom of the foot, has several causes including Tarsal Tunnel Syndrome. Plantar Fasciitis. Heel Spurs.
Symptoms
You might have Retrocalcaneal Bursitis if you notice any of the following symptoms. You have pain or tenderness at the back of the heel where the Achille's tendon attaches. Have swelling near the attachment of the tendon to the heel bone. You have noticed a slowly growing bump on the back of the heel. The back of the heel turns red after getting rubbed in shoes. The back of the heel hurts worse when you run, walk up hill or wear high heels.
Diagnosis
Plain radiographs of the calcaneus may reveal a Haglund deformity (increased prominence of the posterosuperior aspect of the calcaneus). However, on weight-bearing lateral radiographs, the retrocalcaneal recess often appears normal even in patients with retrocalcaneal bursitis, limiting its usefulness in making this diagnosis.Radiographs may be used as a diagnostic measure to support a clinician?s diagnosis of retrocalcaneal bursitis. Individuals with retrocalcaneal bursitis may have an absence of the normal radiolucency (ie, blunting) that is seen in the posteroinferior corner of the Kager fat pad, known as the retrocalcaneal recess or bursal wedge. This may occur with or without an associated erosion of the calcaneus.
Non Surgical Treatment
Orthotics may assist heel bursitis by providing stability to the heel, reduce any foot functioning abnormalities and provide extra support for the feet. The orthotic achieves this by maintaining correct foot posture, therefore facilitating normal functioning of the Achilles tendon. Icing the back of the heel post activity for temporary relief. Non-steroidal anti-inflammatory medication such as ibuprofen can reduce inflammation of the bursa. Stretching of the calf muscle may reduce the pulling on the heel by the Achilles tendon. Shoes that have an elevated heel may reduce pulling on the heel from the Achilles tendon. Resting the painful heel may reduce inflammation and pain. Surgical removal of the painful bursa is a last resort treatment when all other treatments have failed.
Surgical Treatment
Surgery. Though rare, particularly challenging cases of retrocalcaneal bursitis might warrant a bursectomy, in which the troublesome bursa is removed from the back of the ankle. Surgery can be effective, but operating on this boney area can cause complications, such as trouble with skin healing at the incision site. In addition to removing the bursa, a doctor may use the surgery to treat another condition associated with the retrocalcaneal bursitis. For example, a surgeon may remove a sliver of bone from the back of the heel to alter foot mechanics and reduce future friction. Any bone spurs located where the Achilles attaches to the heel may also be removed. Regardless of the conservative treatment that is provided, it is important to wait until all pain and swelling around the back of the heel is gone before resuming activities. This may take several weeks. Once symptoms are gone, a patient may make a gradual return to his or her activity level before their bursitis symptoms began. Returning to activities that cause friction or stress on the bursa before it is healed will likely cause bursitis symptoms to flare up again.
Hammer Toe Surgery Procedures
 Overview
Overview
hammertoe is most common in women, and a big part of this is poor shoe choices, which are a big factor in the development of many foot problems. Tight toe boxes and high heels are the biggest culprits. Genetics certainly plays a role in some cases of hammertoes, as does trauma, infection, arthritis, and certain neurological and muscle disorders. Most cases of contracted toes are associated with various biomechanical abnormalities in how a patient walks. This causes the muscles and tendons to be used excessively or improperly, which deforms the toes over time.
Causes
Medical problems, such as stroke or diabetes that affect the nerves, may also lead to hammertoe. For example, diabetes can result in poor circulation, especially in the feet. As a result, the person may not feel that their toes are bent into unnatural positions. The likelihood of developing hammertoe increases with age and may be affected by gender (more common in women) and toe length; for example, when the second toe is longer than the big toe, hammertoe is more likely to occur. Hammertoe may also be present at birth. Genetics may factor in to developing hammertoe, particularly if the foot is flat or has a high arch, resulting in instability.
 Symptoms
Symptoms
The middle joint of the toe is bent. The end part of the toe bends down into a claw-like deformity. At first, you may be able to move and straighten the toe. Over time, you will no longer be able to move the toe. It will be painful. A corn often forms on the top of the toe. A callus is found on the sole of the foot. Walking or wearing shoes can be painful.
Diagnosis
The earlier a hammertoe is diagnosed, the better the prognosis and treatment options. Your doctor will be able to diagnose your hammertoe with a simple examination of hammertoe the foot and your footwear. He or she may take an x-ray to check the severity of the condition. You may also be asked about your symptoms, your normal daily activities, and your medical and family history.
Non Surgical Treatment
Hammer toes usually get progressively worse over time, especially if you avoid seeking care. Not all cases are the same, so it is important to get your podiatrist or foot surgeon to evaluate your condition so that you can get the treatment you need as soon as possible. Your treatment options will vary depending on the severity of your hammer toe. You may not require surgery to treat your hammer toe. Your doctor may suggest one of these less invasive measures. Instead of wearing shoes that are too high or too short, wear comfortable shoes that have plenty of room and are flat or low-heeled. Your doctor can prescribe pads that will prevent your corns or calluses from getting irritated. Avoid over-the-counter medicated pads, as they contain acid that can worsen your condition. An orthotic device can be customized to fit your shoe and foot. It can help control your tendon and muscle imbalance, which in turn may ease your pain. NSAIDS (nonsteroidal anti-inflammatory drugs) such as ibuprofen can reduce inflammation. By relieving swelling in your toe joint, you can alleviate your pain. Splints or small straps can be placed on your toe by a foot surgeon to realign your bent toe. Applying ice packs wrapped in cloth on your hammer toe can reduce inflammation and swelling. Gently massaging your toes can assist in alleviating your pain caused by hammer toes. Try exercises that stretch your feet as these can help restore your muscle balance. A simple exercise that can help is to pick up a cloth or small object from the floor by curling your toes. This action will help your feet and toes by stretching them.
Surgical Treatment
If you are unable to flex your toe, surgery is the only option to restore movement. Surgery is used to reposition the toe, remove deformed or injured bone, and realign your tendons. Surgery is normally done on an outpatient basis, so you can return home on the day of your surgery.
Hammer Toe Signs Symptoms
 Overview
Overview
A hammer toe can be defined as a condition that causes your toe to bend downward instead of pointing forward. While it can occur on any toe on your foot, it usually affects the second or third toe. If your baby toe curls instead of buckling, it is also considered a hammer toe. There are two types of hammer toes. If your toes still can move around at the joint, then it is considered a flexible hammer toe. It is a milder form of the condition and there are more treatment options. The other type is called a rigid hammertoes, which occurs when the tendons in your toe become so rigid that they push your toe joint out of alignment, and it cannot move at all. Typically, you will need surgery to fix it.
Causes
Medical problems, such as stroke or diabetes that affect the nerves, may also lead to hammertoe. For example, diabetes can result in poor circulation, especially in the feet. As a result, the person may not feel that their toes are bent into unnatural positions. The likelihood of developing hammertoe increases with age and may be affected by gender (more common in women) and toe length; for example, when the second toe is longer than the big toe, hammertoe is more likely to occur. Hammertoe may also be present at birth. Genetics may factor in to developing hammertoe, particularly if the foot is flat or has a high arch, resulting in instability.
A toe stuck in an upside-down "V" is probably a hammertoe. Some symptoms are, pain at the top of the bent toe when putting on a shoe. Corns forming on the top of the toe joint. The toe joint swelling and taking on an angry red colour. Difficulty in moving the toe joint and pain when you try to so. Pain on the ball of the foot under the bent toe. Seek medical advice if your feet regularly hurt, you should see a doctor or podiatrist. If you have a hammertoe, you probably need medical attention. Ask your doctor for a referral to a podiatrist or foot surgeon. Act now, before the problem gets worse.
Diagnosis
Although hammertoes are readily apparent, to arrive at a diagnosis the foot and ankle surgeon will obtain a thorough history of your symptoms and examine your foot. During the physical examination, the doctor may attempt to reproduce your symptoms by manipulating your foot and will study the contractures of the toes. In addition, the foot and ankle surgeon may take x-rays to determine the degree of the deformities and assess any changes that may have occurred.
Non Surgical Treatment
Often padding and taping are the first steps in a treatment plan. Padding the hammer toe prominence minimizes pain and allows the patient to continue a normal, active life. Taping may change the imbalance around the toes and thus relieve the stress and pain. Anti-inflammatory drugs and cortisone injections can be prescribed to ease acute pain and inflammation caused by the joint deformity. Custom shoe inserts made by your podiatrist may be useful in controlling foot function. An orthotic device may reduce symptoms and prevent the worsening of the hammer toe deformity.
Surgical Treatment
Surgical Options: Several surgical procedures are available to the podiatric physician. For less severe deformities, the surgery will remove the bony prominence and restore normal alignment of the toe joint, thus relieving pain. Severe hammer toes, which are not fully reducible, may require more complex surgical procedures. Recuperation takes time, and some swelling and discomfort are common for several weeks following surgery. Any pain, however, is easily managed with medications prescribed by your podiatrist.
Bunions And High Heels
Overview
 A foot bunion is a common cause of foot pain caused by deformity of one of the toe bones. They most commonly affect the big toe, known as hallux abducto valgus, but can also affect the little toe, known as a bunionette. The classic presentation is a large bump on the outer side of the big toe that is red, swollen and painful caused by the toe deviating across towards the second toe. Left untreated, the condition usually gets gradually worse, so it is important to get treatment early on else you may end up needing bunion surgery.
A foot bunion is a common cause of foot pain caused by deformity of one of the toe bones. They most commonly affect the big toe, known as hallux abducto valgus, but can also affect the little toe, known as a bunionette. The classic presentation is a large bump on the outer side of the big toe that is red, swollen and painful caused by the toe deviating across towards the second toe. Left untreated, the condition usually gets gradually worse, so it is important to get treatment early on else you may end up needing bunion surgery.
Causes
Bunions are not inherited, but do tend to run in families. What is inherited is the poor or faulty foot type, that mechanically can lead to the instability around the joint that will eventually lead to bunions, how soon, how quickly and how bad they are or become is assumed to be very dependant on the footwear. A number of other factors are known to play a role in the cause of bunions and hallux valgus. Bunions can follow foot injuries and develop in those with neuromuscular problems. Those with flat feet or pronated feet appear to be more prone to the instability about the joint and have a higher incidence of bunions. Some activities (eg ballet dancing) puts added pressure on the joint and may increase the chance of bunions developing.
Symptoms
Bunions or hallux valgus tend to give pain predominantly from the metatarsal head on the inner border of the foot. The bunion tends to be painful mainly when in enclosed shoes and so is often more symptomatic in winter. As the front part of the foot splays and the great toe moves across towards the 2nd toe a bunion can also produce pain from the 2nd toe itself. The pain which a bunion produces on the 2nd toe is either due to direct rubbing between the great toe and the 2nd toe, a hammer toe type deformity produced due to crowding of the 2nd toe by the bunion and the 3rd toe.The hammer toe will either be painful from its top aspect where it rubs directly on shoe wear or its under surface in the area of the 2nd metatarsal head. This is made prominent and pushed to the sole of the foot by the 2nd toe rising upwards and driving the metatarsal head downwards.
Diagnosis
A doctor can very often diagnose a bunion by looking at it. A foot x-ray can show an abnormal angle between the big toe and the foot. In some cases, arthritis may also be seen.
Non Surgical Treatment
Wide toe box, bunion pads, orthotics, or a combination. Mild discomfort may lessen by wearing a shoe with a wide toe box or with stretchable material. If not, bunion pads purchased in most pharmacies can shield the painful area. Orthotics can also be prescribed to redistribute and relieve pressure from the affected articulation. If conservative therapy fails, surgery aimed at correcting abnormal bony alignments and restoring joint mobility should be considered. If the patient is unwilling to wear large, wider shoes to accommodate the bunion because they are unattractive, surgery can be considered; however, patients should be told that orthotic devices should be worn after surgery to reduce the risk of recurrence. For bursitis, bursal aspiration and injection of a corticosteroid are indicated. For osteoarthritic synovitis, oral NSAIDs or an intra-articular injection of a corticosteroid/anesthetic solution reduces symptoms. For hallux limitus or hallux rigidus, treatment aims to preserve joint mobility by using passive stretching exercises, which occasionally require injection of a local anesthetic to relieve muscle spasm. Sometimes surgical release of contractures is necessary. 
Surgical Treatment
Bunion surgery generally involves repositioning the maligned bones with a bone cut (osteotomy) and/or bone mending procedure (fusion). As such, the time it takes for bones to set or mend in the corrected position generally takes six weeks. Smokers and those in poor medical health may take longer to mend the bone. The biology of bone healing is about six weeks, that time frame can't be made quicker. What can be changed is the disability that one experiences while the bone is mending.
Does Overpronation Necessitate Surgery
Overpronation and underpronation describe general foot movements. These terms do not necessarily describe a medical problem with a foot. For example, you can overpronate and not have any problems or symptoms at all. It is important to have your foot structure and symptoms adequately assessed by your prescribing physician and a qualified practitioner such as a Canadian Certified Pedorthist. Once the underlying conditions and mechanical faults are assessed, an appropriate treatment plan including possible orthotic and footwear recommendations can be made.
Causes
Generally fallen arches are a condition inherited from one or both parents. In addition, age, obesity, and pregnancy cause our arches to collapse. Being in a job that requires long hours of standing and/or walking (e.g. teaching, retail, hospitality, building etc) contributes to this condition, especially when standing on hard surfaces like concrete floors. Last, but not least unsupportive footwear makes our feet roll in more than they should.
Symptoms
Because overpronation affects the entire lower leg, many injuries and conditions may develop and eventually cause problems not only in the leg and foot, but also the knee, hips and lower back. Pain often begins in the arch of the foot or the ankle. Blisters may develop on the instep, or on the inside edge of the heels. As overpronation continues and problems develop, pain will be felt elsewhere, depending on the injury.
Diagnosis
You can test for pronation by looking at the leg and foot from the back. Normally you can see the Achilles Tendon run straight down the leg into the heel. If the foot is pronated, the tendon will run straight down the leg, but when it lies on the heel it will twist outward. This makes the inner ankle bone much more prominent than the outer ankle bone.
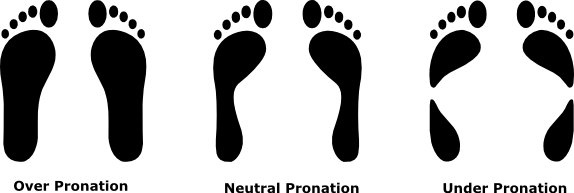
Non Surgical Treatment
When you see the doctor, he or she will likely perform a complete examination of your feet and watch you walk. The doctor will need to take x-rays to determine the cause of your flat feet. In some cases, further imaging may be needed, especially if your symptoms are severe and sudden in nature. Once you are properly diagnosed, your doctor will create an appropriate treatment plan. There are several options to correct overpronation, such as orthotics. In many cases, overpronation can be treated with non-surgical methods and over-the-counter orthotics. In severe cases, however, custom-made orthotics may work better. Orthotics provide arch support and therefore prevent collapse of the arch with weight bearing. They are made of materials such as spongy rubber or hard plastic. Your doctor will also want to examine your footwear to ensure they fit properly and offer enough medial support. Extra support and stability can be achieved with footwear that has a firm heel counter. If you are experiencing pain, you should be able to use over-the-counter pain medications such as ibuprofen to relieve symptoms.
Prevention
Duck stance: Stand with your heels together and feet turned out. Tighten the buttock muscles, slightly tilt your pelvis forwards and try to rotate your legs outwards. You should feel your arches rising while you do this exercise.
Calf stretch:Stand facing a wall and place hands on it for support. Lean forwards until stretch is felt in the calves. Hold for 30 seconds. Bend at knees and hold for a further 30 seconds. Repeat 5 times.
Golf ball:While drawing your toes upwards towards your shins, roll a golf ball under the foot between 30 and 60 seconds. If you find a painful point, keep rolling the ball on that spot for 10 seconds.
Big toe push: Stand with your ankles in a neutral position (without rolling the foot inwards). Push down with your big toe but do not let the ankle roll inwards or the arch collapse. Hold for 5 seconds. Repeat 10 times. Build up to longer times and fewer repetitions.
Ankle strengthener: Place a ball between your foot and a wall. Sitting down and keeping your toes pointed upwards, press the outside of the foot against the ball, as though pushing it into the wall. Hold for 5 seconds and repeat 10 times.
Arch strengthener: Stand on one foot on the floor. The movements needed to remain balanced will strengthen the arch. When you are able to balance for 30 seconds, start doing this exercise using a wobble board.
Physical Rehabilitation And Severs Disease
One of the more common limitations to children enjoying their youthful energy is Sever?s Disease. Sever?s Disease is a pathology that affects the heels of children in their high growth years (usually around 9-15), and it can be quite painful. It usually occurs due to repetitive trauma or impact at the heel. This means that if your child spends a lot of time running around (in sports, or just with friends) the continuous impact of his or her heel to the ground can cause this! Usually, most children will complain of heel pain specifically when they are active; these are considered milder cases. In more severe cases the pain may never cease, whether the child is active or not.
Causes
Sever?s disease is caused by repetitive tension and/or pressure on the growth center of the heel. Running and jumping place a large amount of pressure on the heels and can cause pain. Children with Sever?s may limp or have an altered gait due to the pain. Risk factors for Sever's include tight calf muscles, weak ankle muscles, and alignment abnormalities at the foot and ankle. Sever?s can also result from wearing shoes without sufficient heel padding or arch support.
Symptoms
In Sever?s disease, heel pain can be in one or both heels. It usually starts after a child begins a new sports season or a new sport. Your child may walk with a limp. The pain may increase when he or she stands on tiptoe. Your child?s heel may hurt if you squeeze both sides toward the very back. This is called the squeeze test. Your provider may also find that your child?s heel tendons have become tight.
Diagnosis
Sever condition is diagnosed by detecting the characteristic symptoms and signs above in the older children, particularly boys between 8 and 15 years of age. Sometimes X-ray testing can be helpful as it can occasionally demonstrate irregularity of the calcaneus bone at the point where the Achilles tendon attaches.
Non Surgical Treatment
Please realize that the disorder may last only a couple of weeks to as long as 1-2 years. The treatment plan as prescribed by your doctor MUST be adhered to closely, and the activity level of the child must be controlled during the early stages of treatment. All jumping and running sports, such as basketball, trampoline, volleyball, tennis, soccer, etc., must be eliminated as part of the initial treatment. Once the child has improved and the pain has subsided, a rigid stretching program must then be implemented.
Recovery
One of the most important things to know about Sever's disease is that, with proper care, the condition usually goes away within 2 weeks to 2 months and does not cause any problems later in life. The sooner Sever's disease is addressed, the quicker recovery is. Most kids can return to physical activity without any trouble once the pain and other symptoms go away.